- Emergency Services. TRICARE defines an emergency as a medical, maternity,. Dental emergencies, such as going to the emergency room for a severe toothache, are not a covered medical benefit under TRICARE. Home Health Care. Home health care covers part-time or intermittent skilled.
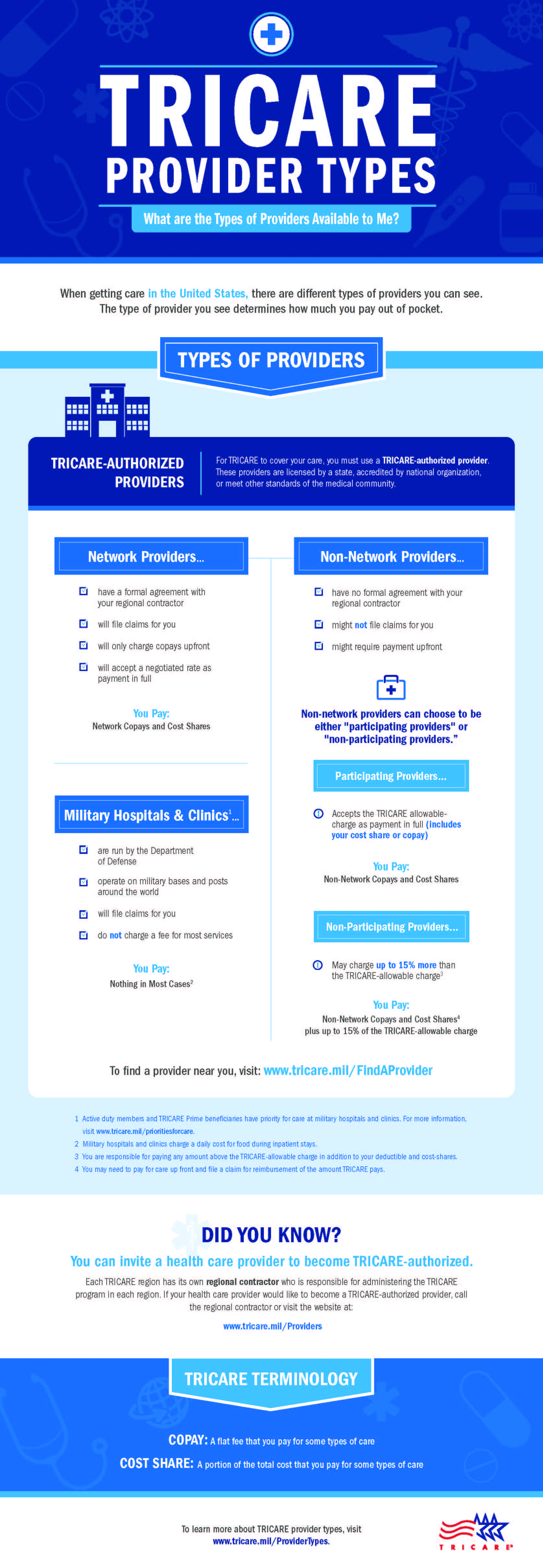
- TRICARE Reserve Select reminders: Beneficiaries may be required to pay up to 15% above the TRICARE allowed amount when using a nonparticipating provider. Annual deductibles apply to outpatient services only.Costs may apply for durable medical equipment (DME) and medications/drugs.
Note: Visit our Copayment and Cost-Share Information page for 2021 costs. View the cost information below for TRICARE Young Adult (TYA) beneficiaries. The amounts are based on the TYA enrollee's sponsor's active duty or retiree status. Copayments are per occurrence or per visit. Cost-shares are a percentage of the contracted rate for network providers and the maximum TRICARE allowable for non-network providers on certain types of services. Beneficiaries have an out-of-pocket maximum for covered medical expenses; this is known as the catastrophic cap.
Covered Services
Learn more about what we cover -including health, dental, and pharmacy.
TRICARE covers emergency care to include professional and institutional charges and services and supplies that are ordered or administered in an emergency department.
Call 911 or Go to the Emergency RoomThe hospital department that provides emergency services to patients who need immediate medical attention.
Make sure you go to an emergency room. Urgent care clinics offer quick walk-in services without an appointment, but these facilities are not considered to be 'emergency rooms.' If you go to an urgent care clinic, make sure you follow your plan's rules for getting urgent care.
Enrolled in TRICARE Prime?
If you're enrolled in a TRICARE Prime plan, contact your primary care manager within 24 hours or the next business day after you receive emergency care.
What is an Emergency?
Examples of emergencies include:
- No pulse
- Severe bleeding
- Spinal cord or back injury
- Chest pain
- Severe eye injury
- Broken bone
- Inability to breathe
See the chart below for more information.
| Type of Emergency | Description |
|---|---|
| Medical | The sudden and unexpected onset of a medical condition or the acute exacerbation of a chronic condition that is:
|
| Maternity | A sudden unexpected medical complication which puts the mother or baby at risk |
| Psychiatric | When the patient is at immediate risk of serious harm to self or others as a result of mental disorder and requires immediate continuous skilled observation at the acute level of care.*
*Based on a psychiatric evaluation performed by a physician or other qualified mental health care professional with hospital admission authority. |
This list of covered services is not all inclusive. TRICARE covers services that are medically necessaryTo be medically necessary means it is appropriate, reasonable, and adequate for your condition. and considered proven. There are special rules or limits on certain services, and some services are excluded.
Last Updated 6/18/2020
Find a Doctor
Prescriptions
Vision
Mental Health Therapeutic Services

Coronavirus (COVID-19) Update:
Providers are expected to refund cost-sharing amounts to beneficiaries as appropriate. |
- TRICARE Select, TRICARE Young Adult Select, TRICARE Reserve Select, and TRICARE Retired Reserve annual deductibles apply.
- TRICARE Young Adult costs are based on the sponsor's status.
- Transitional Assistance Management Program (TAMP) beneficiaries (service members and their family members) follow the active duty family member copayment/cost-share information, based on the TRICARE plan type.
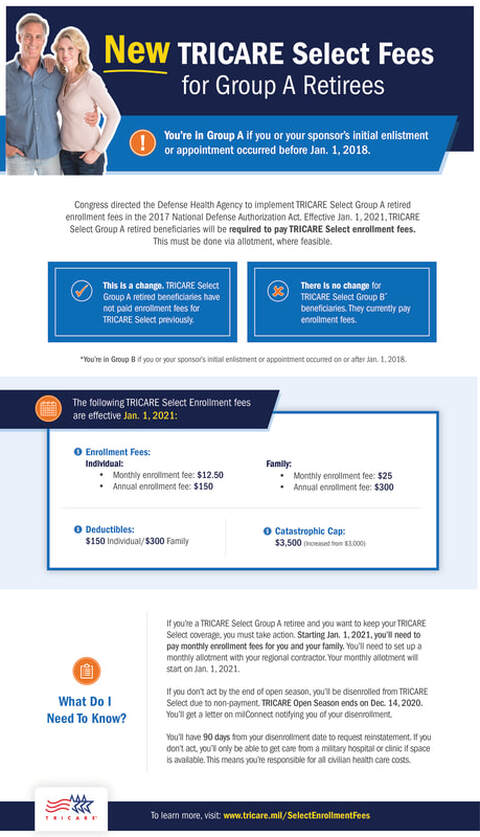
A beneficiary's cost is determined by the sponsor's initial enlistment or appointment date:
- Group A: Sponsor's enlistment or appointment date occurred prior to Jan. 1, 2018.
- Group B: Sponsor's enlistment or appointment date occurred on or after Jan. 1, 2018.
TRICARE Prime and TRICARE Prime Remote (not including TRICARE Young Adult)
| Active Duty Family Members | Retirees and Their Family Members |
|---|---|
Group A: $0 Group B: $0 | Group A: $63 Group B: $63 |
TRICARE Select (not including TRICARE Young Adult)
| Active Duty Family Members | Retirees and Their Family Members |
|---|---|
Group A: Network Provider: $93 Group B: Network Provider: $42 | Group A: Network Provider: $125 Group B: Network Provider: $84 |
TRICARE Reserve Select (TRS) and TRICARE Retired Reserve (TRR)
| TRS | TRR |
|---|---|
| Network Provider: $42 Non-Network Provider: 20% | Network Provider: $84 Non-Network Provider: 25% |

Tricare Prime Er Copay
TRICARE Young Adult (TYA)
Tricare Select Emergency Room Copay List
| TYA Prime | TYA Select | ||
|---|---|---|---|
| Active Duty Family Members | Retiree Family Members | Active Duty Family Members | Retiree Family Members |
| $0 | $63 | Network Provider: $42 Non-Network Provider: 20% | Network Provider: $84 Non-Network Provider: 25% |
